health resources
Resources to support safe, mana-enhancing healthcare for victim-survivors
Our four health resources are below. We welcome your thoughts about their usefulness and any potential improvements: please visit our quick anonymous questionnaire to share your feedback.
For Victim-Survivors Attending Healthcare Appointments: ‘How to Support Me’ Request Template
Healthcare appointments - whether with the dentist, doctor, hospital, nurse, pharmacist, allied professional such as physio or osteopath, traditional carers, alternative carers or others - may be empowering and restoring, but they can also risk creating additional trauma and distress.
This template is for you to edit and give to health practitioners to let them know how to best prioritise your personal, physical, psychological, social and cultural safety.
It is a Microsoft Word document that you can download and adjust by editing, deleting and/or adding to as you wish. If you prefer to use internet apps such as Google Docs, download the MS Word template, then upload it into your own app account for conversion. Any of the wording can be changed to suit your voice or address your needs. After you are finished editing the template you can save it and email it to your health practitioner, or print it out to take with you to your appointment (but note that, depending on your choices, some of the requests may require advance notice to arrange).
We hope this document will help you communicate with healthcare professionals to enable them to support you and safeguard your autonomy and control in healthcare appointments.
Instructions for using the template are included on the first page.
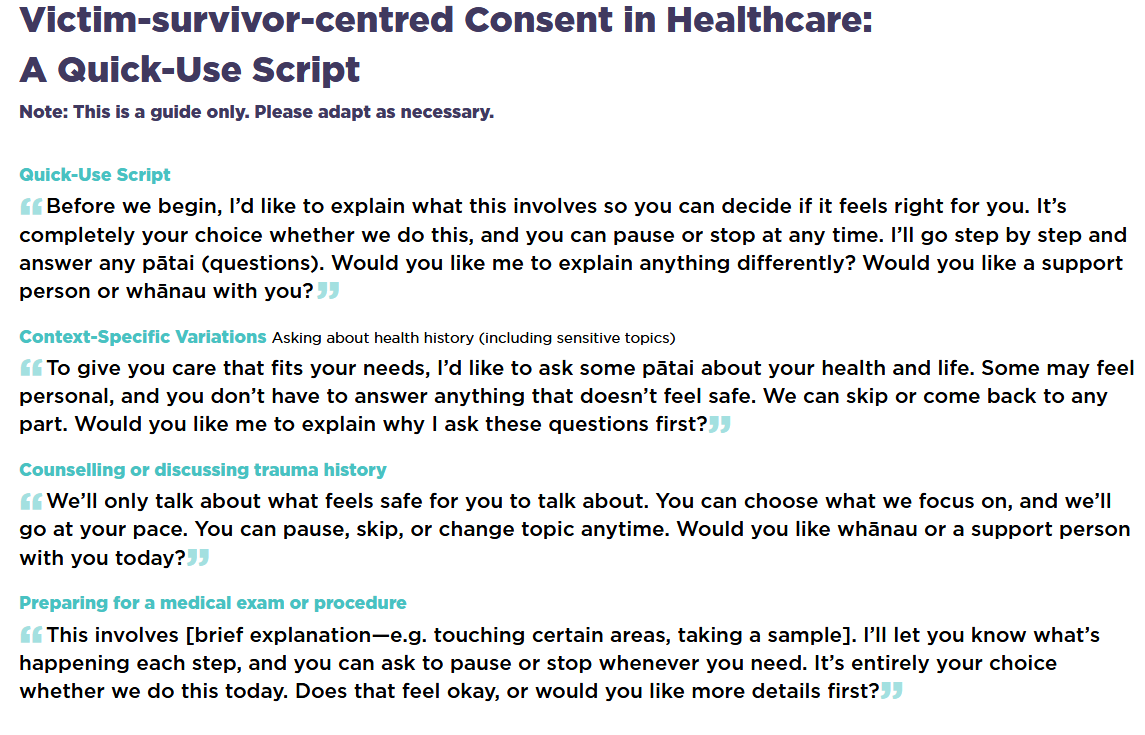
Victim-survivor-centered Consent in Healthcare: A Quick-Use Script
Centering Victim-Survivors in Healthcare Appointments: A guide for Health Practitioners
An informative and practical guide designed for all health practitioners as a reminder about why and how victim-survivors experience trauma reactions, how to better support them, and how to look after themselves during these interactions.
The guide includes a quick script re requesting consent and a one-page summary of things you can do when a patient is distressed.
It also defines family violence and sexual violence, explains what we mean by “trauma”, and how this can affect how patients present. It includes an explanation of the implications for health practitioners when engaging with victim-survivors who may find healthcare appointments difficult due to the trauma they carry, and how to best support such patients with a victim-survivor-centered approach.